News
Find out about the latest research in andrology, urology and sexual medicine2 Simple
Photos: Samir Rodrigues
Due to the COVID-19 pandemic, medical supplies have become scarce. In several countries around the world, such as Italy, the Netherlands and others, there was a lack of equipment to protect healthcare workers. This was reflected in a high rate of contamination of these professionals. In Brazil, we followed the same path.
To try to solve this problem, Dr. Alexandre Miranda was one of the creators of the SOS3DCOVID19 action (www.sos3dcovid19.com.br), together with engineers, professors and university students, to produce personal protective equipment (PPE) voluntarily and free of charge.
Initially, Dr. Alexandre Miranda helped with the production of face shields, created using 3D printing. However, each unit took an average of 2 hours to print. For this reason, Dr. Alexandre Miranda set out to develop a new face shield, created using only PETg. This one has the advantage of being created industrially, on a large scale.
 3D printed Face Shield
3D printed Face Shield
But it wasn't enough just to have a good idea; a significant donation of funds was needed to make large-scale production viable. Dr. Alexandre Miranda then secured a partnership with the COI institute (Centro de Oncologia Integardo - http://institutocoi.org). The latter financed the production of 10,000 units, which were donated to SUS.



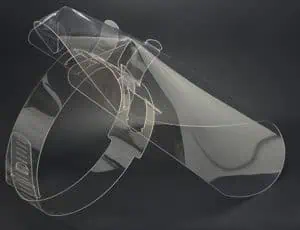
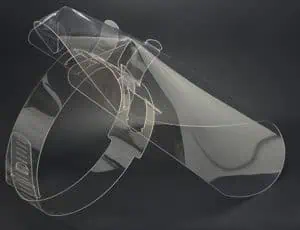
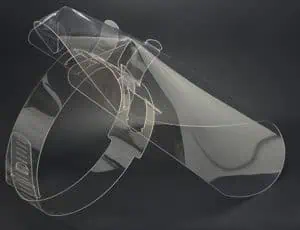



Face Shield 2-Simple (easy to assemble and only 2 pieces)






Donation of the first 2,500 units of the 2 Simple
Vasectomy increases the number of sexual relations
Date: August 31, 2015 / Authors: David P. Guo MD*, Remy W. Lamberts MD and Michael L. Eisenberg MD
Paper published in Journal of Sexual Medicine analyzing the relationship between vasectomy and sexual frequency.
Men who consider having a vasectomy as a form of contraception may be anxious about their future sexual potency. As a result, couples end up opting for other, less effective forms of contraception.
This study tries to find out if there is a relationship between having a vasectomy and the number of times the couple has had sexual intercourse after the procedure.
351 men who had undergone vasectomy were analyzed. The results showed that the number of sexual acts performed by couples after vasectomy was higher than in couples where the man had not had a vasectomy.
The conclusion is that vasectomy makes couples have more sex.
Prostate volume can impact on male sexual function after photoselective vaporization of the prostate (Green Light)
Int Urol Nephrol . 2013;45: 961-966.
In this study, the authors assessed whether the size of the prostate to be operated on could influence the patients' erection. We know that vaporizing the prostate with the Green Light Laser takes a long time when the size of the prostate is large. This means a lot more energy and heat at the ablation site, which can compromise the nerves that cause an erection.
128 patients took part in the study. They were allocated into 2 groups. The first with patients who had an average prostate weight 70g. They completed a validated questionnaire to assess prostate function (IIEF-5) before surgery and up to 2 years later.
After 2 years of follow-up, the group with a prostate < 70g obtained a better quality erection than those with volumes greater than 70g.
This study showed that patients with prostates larger than 70g treated with LASER green light had a negative impact on sexual function (erection) from 6 months onwards.
Clinical Safety and Efficacy of Clostridial Histolytic Collagenase Injection (Xiaflex) in Patients with Peyronie's Disease: Phase 3 Open-Label Study.
Journal of Sexual Medicine. 2015;12: 248-258.
Another good piece on the use of Xiaflex.
347patients took part in the study. They received up to 8 injections of xiaflex and were followed by 36 weeks
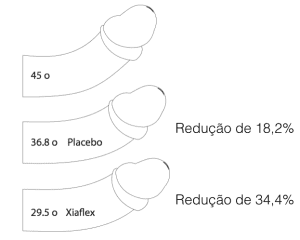
The initial average curvature was 53o. After 36 weeks of follow-up, the final mean curvature was 34.7oThis represents an improvement of 18,3o (or 34,4%) of penile curvature.
We know that the placebo effect (use of saline solution instead of Xiaflex) creates an 18.2% improvement in curvature (Gelbard M, et al. J Urol. 2013 Jul;190(1):199-207). So if we use xiaflex in a patient with 45o of curvature he will have a final result of 29,5o deviation (improvement of 34,4%). If we use saline (placebo) instead of xiaflex, the result will be 36,8o deviation (improvement of 18,3%). To help visualize the result Xiaflex vs. Placebo I'll put an image of the results previously quoted at the end of this text.
As can be seen in the figure below, the use of Xiaflex doesn't seem to have made such a big difference to the placebo. Although there is strong scientific evidence that Xiaflex works better than placebo, I don't think it effectively rectifies penile curvatures, especially in more severe cases (> 60o).
We must also remember that the medication is expensive. In the United States, each dose costs an average of $3,300.00 per application. This means that in 8 applications the final cost of the treatment will be $ 26,400.00.
The medication has not yet been released for use in Brazil.
Phase II Randomized Trial Evaluating Erectile Function after Attempted Cavernous Nerve Sparing with Unilateral Sural Grafting versus No Sparing in Radical Prostatectomy for Clinically Localized Prostate Cancer
European urology. 2009;55: 1135-43.
An important study of excellent quality to evaluate the effectiveness of erection recovery after surgery for prostate cancer, using a sural nerve graft (from the side of the leg) to "reconnect" the nerve that generates the erection.
107 patients took part in the study. They were assigned to 2 groups. The first received the sural nerve graft (66 patients) and the second did not (41 patients).
After 2 years of follow-up 71% of the patients who received the graft had an adequate penile erection; while in the group that did not receive the graft the number was 67%.
This study shows that there is no improvement in erection with this surgery in patients, in addition to the increase in surgical time (The average time to place the graft is 164 minutes).
Clinical efficacy, safety and tolerability of histolytic clostridial collagenase (xiaflex) in the treatment of Peyronie's disease in 2 large double-blind, radomized, controlled, phase 3 studies.
J Urol. 2013 Jan 30. pii: S0022-5347(13)00227-9. doi: 10.1016/j.juro.2013.01.087. [Epub ahead of print]
Another study published using xiaflex. Preliminary results continue to show that it does very little to resolve penile tortuosity.
The patients were divided into two groups in this study. One group received an injection of xiaflex into the penis and the other received an injection of saline (placebo).
The group that received xiaflex had an average tortuosity of 50,1After 52 weeks of treatment (8 applications) they had a curvature of 33,1The individuals in the second group had an initial tortuosity of 49,3At the end of the treatment she was 40o.
The conclusion is that xiaflex only reduces 7,7after 52 weeks of invasive treatment, when compared to placebo.
It was noted that 84.2% of the patients who used xiaflex had a local adverse reaction, such as pain, redness, bruising, swelling, etc.
Of the 558 patients treated with the drug, 3 had to undergo emergency surgery due to rupture of the tunica albuginea (inner part of the penis), which had been eroded by the medication.
The impression we get at the end is that it's a drug that causes a lot of side-effects and has low resolutivity, as it only rectifies 7,7compared to placebo.
Psychological impact of Peyronie's disease - Review
This review was published in the Journal of Sexual Medicine (J Sex Med. 2012 Nov 15) and talks about the psychological impact of peyronie's disease.
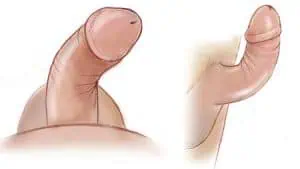
Peyronie's disease is a complex illness that generates a curvature deformity in the penis, producing negative physical and psychological effects for the patient. Depression, erection difficulties and emotional relationships are commonly affected in men with the disease.
The challenges imposed by Peyronie's disease include changes in the sexual relationship, restriction of intimacy, depression, social isolation and stigmatization. All are linked and reinforced by each other.
It is important for the doctor to recognize these associated psychosocial alterations and know how to actively access them, both with the patient and the partner, in order to improve quality of life and promote appropriate treatment for this patient.
Intratumoral Injection of Adipose Tissue-Derived Stem Cells Prevents Fibrosis and is Associated with Improved Erectile Function in a Rat Model of Peyronie's Disease.
A study published in European Urology showed that the use of stem cells, when injected into the tunica albuginea (penis), prevents fibrous formation and the degradation of elastic fibers in the corpus cavernosum, which leads to Peyronie's disease. The idea is that, in the future, this treatment can be used on patients who start the disease, i.e. in the acute phase, preventing the disease from appearing.
Effect of tunica defect size after Peyronie's plaque excision on postoperative erectile function: Do centimeters really matter?
Interesting paper, published in the journal UROLOGY (Urology. 2012 Nov;80(5):1051-5).
The author concludes that plaque excision and skin grafting should only be recommended for Peyronie's disease patients with good erectile capacity, with a large deviation (which cannot be corrected by plication alone), for patients who do not accept any shortening of the penis and if the size of the tunica defect (penis) is < 3cm. A defect of 3 cm should not be exceeded, as the larger the defect, the greater the chance of erectile dysfunction.
This study is yet another in the literature that demonstrates the need to reduce the area of the graft in order to also reduce the chance of losing penile rigidity in the post-operative period.
Peyronie's Disease: Still a Surgical Disease
Article published in ADVANCES IN UROLOGY (Adv Urol. 2012; 2012: 206284).
To date, there is no high-level, evidence-based data to suggest the best surgical treatment for Peyronie's disease. The choice of the perfect treatment should be determined by a two-way conversation between the urologist and the patient, taking into account the severity of the disease, the patient's preference and the surgeon's comfort. There are studies comparing different surgical modalities but the results are not consistent. Major problems include the lack of a standardized training regime, facilitating teaching; the low incidence of the disease, meaning that few doctors are able to accumulate extensive experience in the subject. In our opinion, surgical treatment is currently the only treatment modality that provides an acute and satisfactory result for the deformity associated with Peyronie's disease.
Phase 2b clinical efficacy and safety study of clostridial histolytic collagenase (xiaflex) in patients with Peyronie's disease
Study published in the Journal of Urology (J Urol. 2012 Jun;187(6):2268-74) showing the results of using xiaflex.
It was seen that the injection of xiaflex, without any other mechanical intervention, did not result in an improvement in curvature. Only in the group in which xiaflex was injected + modeling (mechanically forcing the penis to the opposite side) was there an improvement of 11 degrees at the end. This was a percentage improvement of 29.7% on the original curvature.
This study shows what was already known. That xiaflex is not a panacea that will solve the problem of patients with Peyronie's disease. It may be a solution for patients who have a small deformity, something less than 20-30 degrees of deviation.
I see many patients misinformed about xiaflex, thinking it's the solution to their problems. It's a common comment when patients arrive for their consultation.